Wound Wellness Approach
At Wound Wellness, we understand that pressure injury treatment requires not only expert wound care but also comprehensive prevention strategies to protect against future skin breakdown. Our nurse practitioners have specialized training in pressure injury assessment, staging, and treatment, providing evidence-based care that promotes healing while addressing all contributing factors. We offer both in-office and mobile services throughout Lake Villa, Lindenhurst, Grayslake, and surrounding Lake County communities, bringing specialized care directly to patients with mobility limitations. Our approach includes wound treatment, caregiver education, and coordination with other healthcare providers to ensure comprehensive care that addresses all aspects of pressure injury prevention and management.
If you're concerned about pressure injury development or need expert treatment for existing wounds, specialized help is available. Contact Wound Wellness today to schedule a comprehensive evaluation with our experienced pressure injury specialists. We'll assess your situation, provide stage-appropriate treatment, and work with you and your caregivers to develop effective prevention strategies. With our expertise in pressure injury care and convenient service options throughout Lake Villa and Lake County, expert treatment and prevention support are more accessible than ever. Call us at (224) 215-6242 or use our online appointment request form to protect your skin health and promote healing.
Condition at a glance
Pressure Injuries
Pressure injuries develop when prolonged pressure, friction, or shear forces compromise blood flow to skin and underlying tissues. This commonly occurs over bony prominences like the tailbone, heels, hips, shoulders, and back of the head, where there's less protective tissue between bone and skin. Risk factors include immobility, prolonged bed rest, wheelchair use, poor nutrition, dehydration, incontinence, altered mental status, and certain medical conditions that affect circulation or sensation. Older adults, individuals with spinal cord injuries, and patients with chronic illnesses are at particularly high risk. The pressure threshold and duration needed to cause tissue damage varies among individuals, but wounds can begin developing in as little as 30 minutes to two hours of unrelieved pressure.
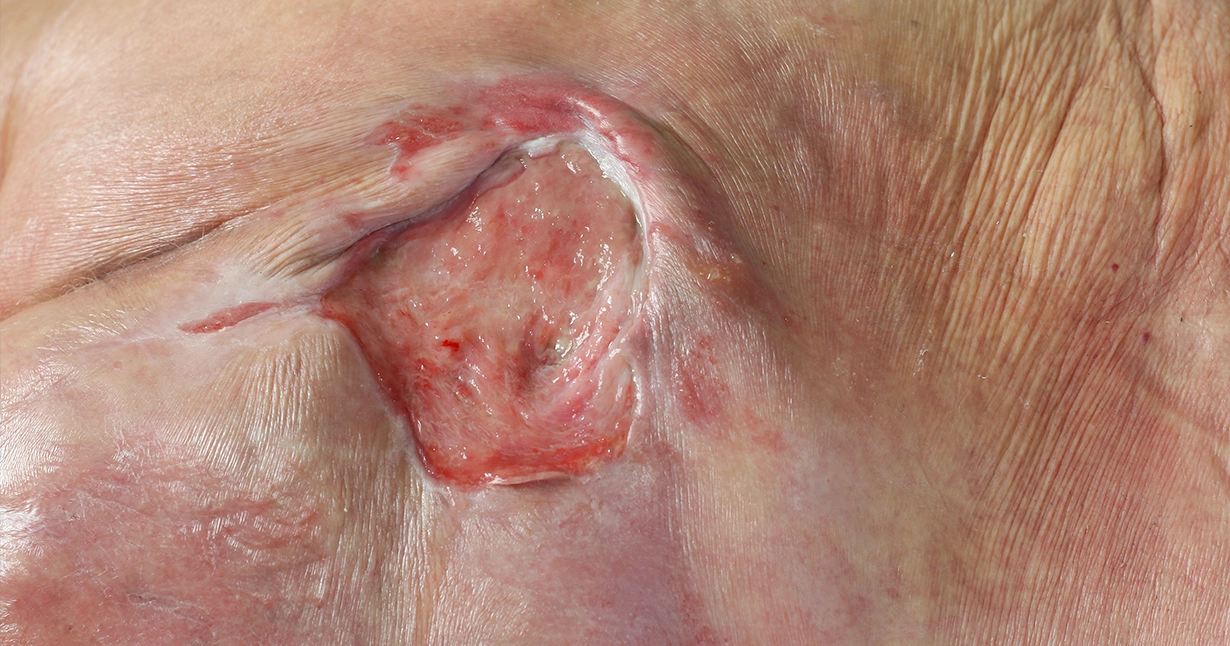
Pressure injuries are classified into stages based on the depth and extent of tissue damage. Stage 1 injuries appear as persistent redness over a bony prominence that doesn't blanch (turn white) when pressed, indicating damaged blood vessels beneath intact skin. Stage 2 injuries involve partial-thickness skin loss, appearing as shallow, open wounds or intact blisters. Stage 3 injuries extend through the full thickness of skin, exposing fat tissue but not bone or muscle. Stage 4 injuries are the most severe, with full-thickness tissue loss exposing bone, muscle, or tendons. There are also unstageable injuries where the wound base is covered by dead tissue, and suspected deep tissue injuries that appear as purple or dark red areas indicating damage to underlying tissues.
Our treatment approach for pressure injuries depends on the stage and specific characteristics of each wound, but always includes addressing the underlying cause—pressure relief. We begin with comprehensive assessment of the wound, surrounding skin, and factors contributing to pressure injury development. Treatment includes appropriate wound cleansing, debridement when necessary, and moisture-balanced dressings that promote healing while protecting healthy tissue. Equally important is implementing pressure redistribution strategies through repositioning schedules, specialized support surfaces, and protective devices. We also address nutritional needs, manage moisture from incontinence, and provide education to patients and caregivers about prevention strategies that reduce the risk of new pressure injuries developing.
When to Seek care
Seek immediate medical attention for any area of persistent redness over a bony prominence that doesn't fade within 30 minutes of pressure relief, as this may indicate the beginning of pressure injury development. Don't wait if you notice any open wounds, blisters, or areas of skin breakdown, especially over pressure points like the tailbone, heels, or hips. Emergency care is needed for signs of infection including fever, increasing pain, foul-smelling drainage, redness extending beyond the wound borders, or red streaking. If you have an existing pressure injury that suddenly worsens, develops unusual drainage, or shows signs of deep tissue involvement, contact your healthcare provider promptly for evaluation.
Prevention Management
Preventing pressure injuries requires consistent attention to pressure relief and skin care, especially for individuals with limited mobility. Establish a regular repositioning schedule—every two hours for bed-bound individuals and every 15-30 minutes for wheelchair users, or more frequently if skin shows signs of pressure damage. Use appropriate support surfaces such as pressure-redistributing mattresses or cushions designed for your specific needs and risk level. Keep skin clean and dry, using gentle cleansers and moisturizers to maintain skin integrity. Check skin daily for signs of pressure damage, paying special attention to bony prominences and areas where medical devices contact the skin. Address incontinence promptly and use protective barriers when needed to prevent moisture-related skin breakdown.
Preventing pressure injuries requires consistent attention to pressure relief and skin care, especially for individuals with limited mobility. Establish a regular repositioning schedule—every two hours for bed-bound individuals and every 15-30 minutes for wheelchair users, or more frequently if skin shows signs of pressure damage. Use appropriate support surfaces such as pressure-redistributing mattresses or cushions designed for your specific needs and risk level. Keep skin clean and dry, using gentle cleansers and moisturizers to maintain skin integrity. Check skin daily for signs of pressure damage, paying special attention to bony prominences and areas where medical devices contact the skin. Address incontinence promptly and use protective barriers when needed to prevent moisture-related skin breakdown.
Treatment Options
Our pressure injury treatment is individualized based on wound stage, location, and patient-specific factors. Treatment may include gentle cleansing, debridement to remove dead tissue, specialized dressings that maintain optimal moisture balance, and advanced therapies such as negative pressure wound therapy for deeper wounds. We coordinate pressure redistribution strategies including appropriate support surfaces, positioning aids, and repositioning schedules. For complex wounds, we may recommend skin substitution therapy or other advanced treatments. Throughout treatment, we work closely with patients, families, and caregivers to ensure proper wound care techniques and effective prevention strategies.